Professor Focuses on Translating Biomaterial Engineering Tools into Nano and Regenerative Medicine
October 2022
By Kathleen Snoeblen
Like his two brothers, Mehdi Razavi was all set to be a materials engineer and get a good job at a large fabrication company after college. But then, he got the news. “My mother was diagnosed with cancer,” he said. During his last year as an undergraduate at Isfahan University of Technology, he took her to the hospital for her treatment, where he saw others with cancer, even children. “And I started to really think about how my materials engineering could apply to the real world, to hospitals and helping patients,” he said. “Not only cancer patients, but also others who are suffering. So I became very interested in biomaterials.
“My mother, thank God, is well now, after her treatment, but that event was something that I became passionate about. The translation of engineering tools to medicine.”
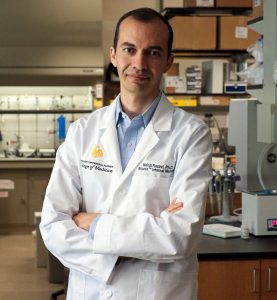
From there, Razavi got his master’s and doctoral degrees and went into biomaterial research. He is now an assistant professor of medicine and a team member of the Biionix (Bionic Materials, Implants & Interfaces) Cluster at UCF. Razavi heads the Biomaterials and Nanomedicine Lab at the College of Medicine and has been there since 2019. Before that, he was a postdoctoral research fellow in regenerative medicine at Stanford University School of Medicine.
“I came to UCF because I found a very collaborative environment between departments,” Razavi said. “My research, because it’s bioengineering, is more multidisciplinary and requires working between different departments, including medicine and engineering,” he said. “Some of the experiments and equipment that I needed to do my research were in the Advanced Materials Processing and Analysis Center (AMPAC) and the NanoScience Technology Center. So these together actually provided a good, top-working environment, which is very hard to find in other institutes.” Razavi also said that Orlando’s Medical City offers opportunities to collaborate with clinicians and scientists at the adjacent Orlando Veterans Affairs Medical Center and Nemours Children’s Health as well as the UCF Lake Nona Hospital.
As part of the Biionix Cluster, Razavi leads two research projects that involve two areas of biomaterials and nanomedicine. One is investigating the manufacture of bioresorbable magnesium implants. “Magnesium is mechanically stronger than biopolymers, very flexible compared to bioceramics, and also resorbable compared to other biometals,” he said. Oftentimes, bone fractures today are surgically fixed with titanium alloy or stainless steel bone plate screws. “Those work well, but the problem is that they require a second surgery to remove. So we want to develop bioabsorbable implants made from magnesium.”
At the Biomaterials and Nanomedicine Lab, Razavi and his team also focus on developing theranostic tools that can be used for diagnostics and therapeutics. “We are trying to find approaches that could be globally deployed, are non-invasive, widely available, portable, and inexpensive,” Razavi said. One of the tools they’ve developed is a technology that uses nanobubbles for different biomedical applications including drug/gene delivery systems.
Ultrasound-Responsive Nanobubbles for Osteoporosis Treatment
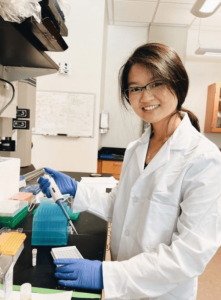
The new technology developed by Razavi and UCF student Angela Shar is a unique nanoplatform for treating osteoporosis, a disease marked by an imbalance between the body’s ability to form new bone tissue (ossification) and break down or remove old bone (resorption). Razavi explained that a healthy body continually replaces old or damaged
bone tissue at a steady rate to ensure good bone quality and mass. “But when the rate of bone resorption becomes higher than bone formation, then it leads to a systemic disease of the skeletal system called osteoporosis,” he said. “Osteoporosis affects more than 10 million Americans, and over 44 million have low bone density, putting them at the risk of bone fracture.”
According to the Bone Health & Osteoporosis Foundation (BHOF), studies suggest that one in two women and up to one in four men age 50 and older will break a bone due to osteoporosis. Also, experts predict that by 2025, osteoporosis will be responsible for about 3 million fractures and $25.3 billion in costs annually. Many osteoporosis treatments to
day use drugs such as bisphosphonates to inhibit bone resorption. Side effects can include jaw osteonecrosis (delayed healing of the jawbone) and gastrointestinal problems.
A viable, safe alternative, the UCF invention both treats and prevents the effects of osteoporosis. “It is a dual-acting technology,” said Razavi. “On one side, you are reducing bone resorption, and on the other side, you are increasing bone formation using ultrasound.” The invention uses ultrasound-responsive nanobubbles to deliver treatment to targeted areas of a person’s body.
“There are a lot of nanoplatforms out there for osteoporosis treatment,” Razavi said. “But the advantage of ultrasound-responsive nanobubbles is that they require ultrasound for bubble disruption and gene delivery. Ultrasound itself can actually facilitate bone formation.”
In one example application, the nanobubbles carry the osteoporosis-related silencing or knockdown gene, Cathepsin K small interfering ribonucleic acid (CTSK siRNA). Razavi said that the nanobubbles both protect the siRNA from directly interacting with its surroundings and targets osteoclast cells, which are the bone cells that carry the CTSK gene. CTSK is a key player in the bone resorption process. “So, we downregulate, reduce high expression of those [bone resorption] genes using the siRNA,” he said.
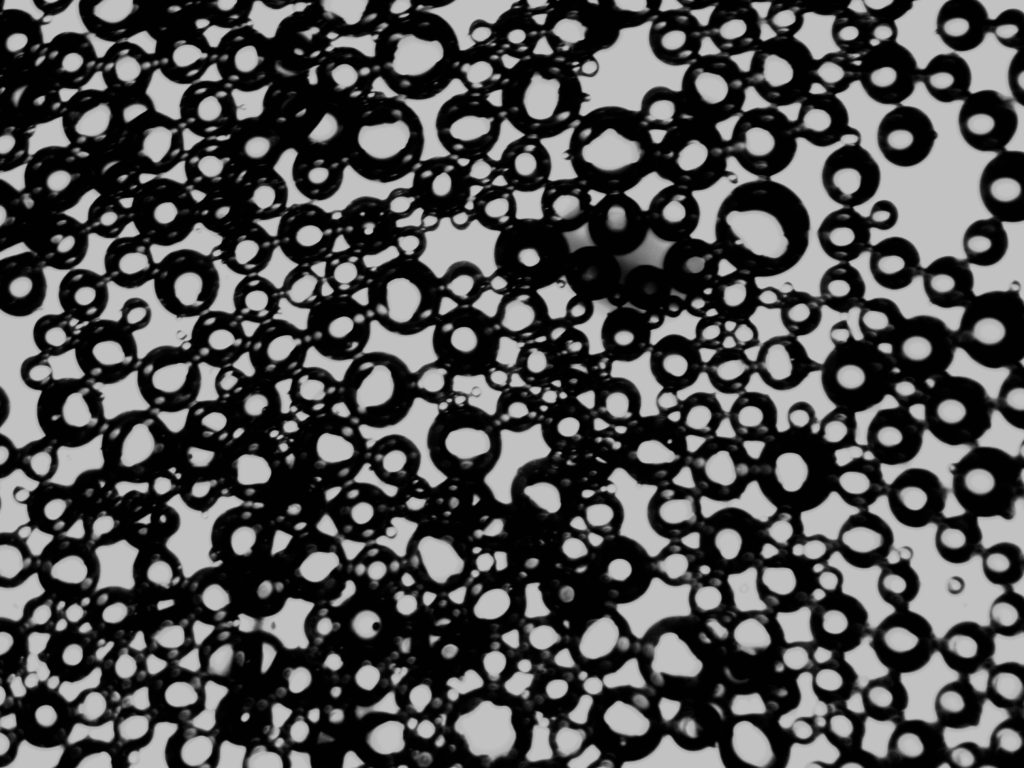
Figure 3. Microscopic image of nanobubbles stimulated with ultrasound, produced at the UCF Biomaterials and Nanomedicine Lab.
He added that the delivery system also helps to slow the release of the treatment and prolong the gene silencing mechanism’s effectiveness.
Each nanobubble encapsulates the treatment in a gas core and liquid shell made from perfluorocarbon. “The gas core helps us to image and track the nanobubbles. It’s also embedded with molecules that can target bone,” said Razavi. “The bubbles go into the bone cells, search and find those genes that cause osteoporosis, and they bury the CTSK siRNA which then creates a complex,” he said. “That complex is thermodynamically unstable, and that will lead to a kind of downregulation or silencing of those genes. When you measure for Cathepsin K expression, you get a lower expression of that.” For controlled, sequential release and customized treatment (for example, low intensity for superficial fractures versus high intensity for deep lesions) the ultrasound parameters can be modified, including exposure time, intensity, frequency, and waveform.
Razavi cited other uses for the invention. “You can use this for cancer and other applications, like neurodegenerative diseases such as Alzheimer’s,” he said. One advantage of nanobubbles over microbubbles is their ability to pass through the cell membrane to deliver therapeutics. “Ultrasound can actually open up the blood-brain barrier to facilitate the migration of the nanobubbles into the neural cells for gene delivery.” Chemo-therapeutic drugs can be encapsulated into the bubbles and then injected to target tumors. Also, because these bubbles have a gas core, they can deliver oxygen. “One solution here is to deliver oxygen into the tissue to facilitate regeneration,” he said.
For more information about the invention, see the technology sheet.
Technology Available for License
To learn more about Razavi’s work and additional potential licensing or sponsored research opportunities, contact Benjamin Neymotin (benjamin.neymotin@ucf.edu) at 407.823.0665.